A 45 year old female with seizures
2K17BATCH
This is an E logbook to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This E-logbook also reflects my patient-centered online portfolio and your valuable inputs in the comments are welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE DETAILS:
A 45 year old female resident of Nalgonda presented to the casualty ward on 9th June 2021 at 4:30 pm with the chief complaints of involuntary movements of all 4 limbs on day 1, dimunition of vision and dizziness since 3 days
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 3 days back then she developed dimunition of vision and dizziness since 3 days.
On 08-06-21 i.e yesterday night she had 1 episode of vomiting followed by 2 episodes of seizures- involuntary movements involving all 4 limbs lasting for 5 minutes ; initially involving right upper limb and lower limb followed by left upper limb and lower limb. Focal with secondary generalization. There was loss of consciousness, tongue bite and frothing.
No history of involuntary passage of stools/micturition.
Postictal confusion for 10 minutes.
Followed day morning i.e on 09-06-21 she had another episode of seizures and was taken to a local hospital where CT was done which showed infarcts in bilaterally.
Again she had 2 episodes of seizures there and then she was referred to our hospital for further treatment.
PAST HISTORY:
A Known case of Hypertension since 10 years
Diabetes mellitus since 10 years, Hypothyroidism since 3 years.
PERSONAL HISTORY:
Married
Diet: Mixed
Appetite: Normal
Bowel and bladder movements: Regular
Micturition: Normal
No addictions
No known allergies
FAMILY HISTORY:
History of Hypertension and Diabetes mellitus in family.
DRUG HISTORY:
History of
Tab. GLICLAZIDE 80 mg OD for Diabetes mellitus since 10 years
Tab. ATEN 50 mg OD for Hypertension since 10 years.
Tuberculosis treatment
GENERAL EXAMINATION:
The patient was examined in a well lit room with informed consent.
Patient was conscious, coherent and cooperative, well oriented to time, place and person.
Pallor : Absent
Icterus: Absent
Cyanosis: Absent
Clubbing of fingers/toes: Absent
Lymphadenopathy : Absent
Edema of feet : Absent
No dehydration
No malnutrition
VITALS:
At the time of admission:
Temperature : Afebrile
BP - 120/70 mmHg
PR- 86 bpm
SPO2 at room air 99% /at 21 litres of oxygen
SYSTEMIC EXAMINATION:
CVS :
S1 and S2 heard
No added thrills and murmurs
RESPIRATORY SYSTEM:
No Dyspnea
No Wheeze
Position of trachea - central
Vesicular breath sounds were heard
No Adventitious sounds
ABDOMEN:
Shape of abdomen: Scaphoid
Tenderness: non tender
No palpable mass
Hernial orifices are normal
No free fluid present
No bruits
Liver is not palpable
Spleen not palpable
Bowel sounds are heard
CNS:
Level of consciousness: conscious
Speech: normal
Signs of meningial irritation:
-Neck stiffness- absent
-Kerning's sign- absent
Cranial nerves: intact
Extensor plantar reflex on one side.
Motor system:
Right. Left
Bulk normal. normal
Tone UL. normal. normal
LL. normal. hypotonic
Power. Right. Left
UL. 4+/5. 4-/5
LL. 4+/5. 3/5
Reflexes:
- Superficial reflexes
Right. Left
Corneal. Present. Present
Conjunctival. Present. Present
Abdominal. Present. Present
Plantar. Withdrawal Extensor
-Deep tendon reflexes
Right. Left
Biceps. + +
Triceps. + +
Supinator. + +
Knee + -
Ankle. + -
jaw jerk +
Glasgow scale: 15/15
No Involuntary movements
SKIN:
Normal
EXAMINATION OF ENT:
Normal
EXAMINATION OF TEETH AND ORAL CAVITY:
Normal
EXAMINATION OF HEAD AND NECK:
Normal
INVESTIGATIONS:
GRBS : 569 mg/dl
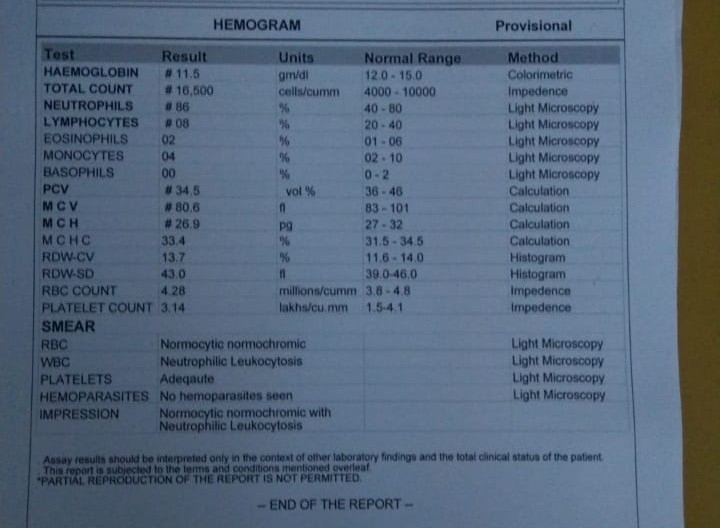
HEMOGRAM:
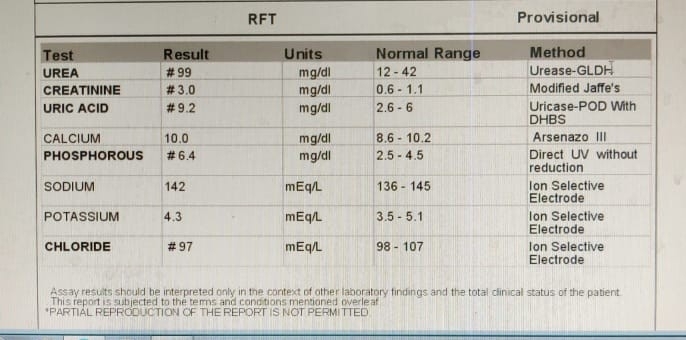
RFT
ABG
SERUM BILURUBIN
URINE FOR KETONE BODIES
PROVISIONAL DIAGNOSIS:
SEIZURES ( FOCAL WITH SECONDARY GENERALIZATION )
2° TO ? CVA OCCIPITAL LOBE INFARCT
? METABOLIC DIABETIC KETOACIDOSIS
LEFT HEMIPARESIS
TREATMENT:
1. INJ. LEVIPIL 1 gm / IV / stat / in 100 ml normal saline
INJ. LEVIPIL 500mg/ IV/BD
2. INJ. HAI 0.1 IU/kg /IV / stat
INJ. HAI 1ml in 39ml NS @6ml/hr till GRBS<70mg/dl
3. INJ. MIDAZOLAM 2CC/IV/ SOS
4. IV FLUIDS - 0.9% / NS CONTINUOUS INFUSION @ 150 ml/hr
5. TAB. THYRONORM 25 mcg/ OD
1---X---X
6. W/F SEIZURE EPISODE
7. TAB. ECOSPIRIN- AV 75/20 mg OD
X---X---1
8. TAB. CLOPITAB 75 mg OD
9. MONITOR BP, PR, TEMPERATURE, SPO2
10. STRICT I/O CHARTING
11. GRBS MONITORING HOURLY
Thank you Dr.Rakesh Biswas sir for this opportunity







Comments
Post a Comment